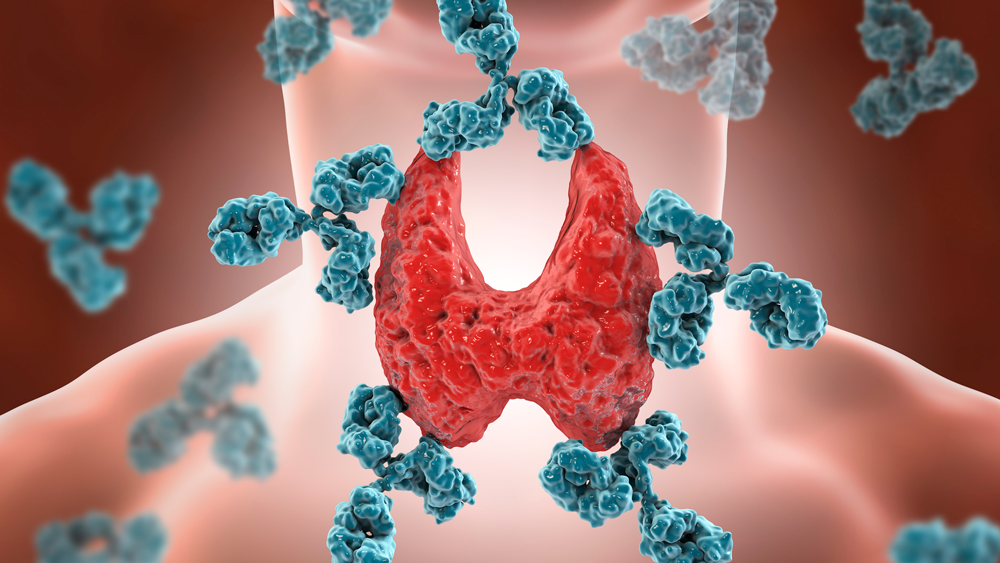
It is an autoimmune disease in which the body’s immune system inadequately affects the thyroid tissue. This condition is believed to have a genetic basis. Hashimoto’s is 5 to 10 times more common in women than in men. People with this disease may have other autoimmune diseases such as pernicious anemia (vitamin B12 deficiency) or type 1 diabetes mellitus.
What is Hashimoto’s thyroiditis?
Hashimoto’s thyroiditis, or autoimmune thyroiditis, or chronic lymphocytic thyroid disease, is one of the most common thyroid diseases. Hashimoto’s is a form of thyroiditis whose cause is not yet fully known; the existence of genetic predisposition, but also environmental factors (toxic substances, excess iodine or even infections).
Hashimoto’s is associated with other autoimmune diseases: insulin-dependent type 1 diabetes, adrenal insufficiency, Biemermer anemia, rheumatoid arthritis, dermatomyositis, myasthenia gravis, vitiligo, etc.
- Symptoms of Hashimoto’s thyroiditis:
The main sign of this disease is an enlarged thyroid gland that has a gummy aspect and develops gradually over several months.
Functional evolution can be:
Hypothyroidism -15%
Hyperthyroidism – 5%
Euthyroiditis (Normal thyroid function) -80%. - Preclinical tests confirming the diagnosis:
Dosage of Ab-TG and Ab-TPO antibodies
Dosage of hormonal balance TSH, FT4, FT3
Echography of the thyroid gland
Protein electrophoresis – hypergammaglobulinemia
Treatment
Corticosteroids are often used to treat autoimmune diseases, but for Hashimoto’s thyroiditis, corticosteroids are not effective. Forms of hyperthyroidism are treated with synthetic antithyroid drugs (ATS). In cases where the volume of the thyroid gland increases or compression occurs or in case of suspicious diagnoses (lymphoma or thyroid cancer) a thyroidectomy is performed.